Free Sample – Unit 1: Cauda equina syndrome presenting as low back pain and sciatica (Preview)
Please note:
The following sample is the first unit in the course called “Recognizing Serious Disorders Masquerading as Mechanical Musculoskeletal Pain – Volume 1”.
Unit Credit: 1 Hour
1 hour includes allocated time for progressing through the learning material and completing the quiz.
Video Playback: If videos don’t play, it’s usually because you’ve remained on this web page for too long or you have lost Internet connection. To resolve this, “refresh” or “reload” this web page and you should then be able to play the videos again.

A Problem-Solving Exercise in History Taking and Physical Examination
The learning material in this unit is designed to improve your skills in history taking and physical examination. The material includes an example of clinical findings and their analysis using a problem-solving approach. As you read through the material and watch the videos, you are encouraged to identify whether all the required elements of history taking and physical examination have been adequately covered.
Taking the Patient’s History
When taking the patient’s history, the practitioner needs to obtain sufficient information to cover the following essential elements:
• Who is the patient?
• Where is the pain?
• When was the onset?
• What caused the onset?
• What are the pain characteristics?
• What are the aggravating and relieving factors?
• What has been the course of the pain?
• Are there any associated symptoms?
• Is there a past history that is relevant to the current complaint?
• Are there any “red flags”?
• What is the list of possible causes for the patient’s complaint?
Who is the patient and where is the pain?
When was the onset and what caused the onset?
Your patient is a 38-year-old carpenter who presents with a primary complaint of severe low back pain. He says that it began 2 days ago when he was lifting a heavy kitchen cupboard into place. The pain came on suddenly and was so intense that it caused him to drop the cupboard to the floor. Within a day, he developed pain and numbness in both legs.
Analysis: This is a case of acute and severe low back pain due to a recent work-related injury. His occupation makes him vulnerable to muscular and joint injuries in the lumbar spine. The accompanied pain and numbness in both lower extremities is of serious concern. Pain in the lower lumbar region and lower extremities is common and can indicate a number of conditions, including:
• Disc injury
• Vertebral motion segment dysfunction
• Sacroiliac joint dysfunction
• Myofascial pain syndromes (e.g, piriformis trigger point referral)
• Muscle strain (e.g., the erector spinae)
• Piriformis syndrome
The development of the lower extremity symptoms within 24 hours of the onset of low back pain suggests a causal relationship. Lumbar disc herniation typically presents with low back pain and begins to abate after the first 24 hours while radiculopathy develops and becomes predominant. Practitioners should always be wary of other causes of pain including serious conditions such as fractures, infections and tumors.
Patient Education Resource
For your convenience, you may download or print the following patient education resource for your practice.
Click here to download the image below.
© All rights reserved.
What are the pain characteristics?
What are the aggravating and relieving factors?
What has been the course of the pain?
He describes his low back pain as sharp and intense, rating it as a 9 out of 10 in intensity. He explains that he can’t stand or sit for too long as this makes the back and lower limb symptoms worse. The anti-inflammatory tablets that he has taken for previous bouts of back pain have not provided any relief this time. He says that lying in bed eases the back pain but does not completely relieve it. He is in so much pain that he asks if he can lie down for the rest of the case history.
Analysis: The severity of the pain is of concern, although the patient’s rating is subject to various factors.
The inability to stand or sit for any length of time because of a worsening in both the lower back and lower extremity symptoms suggests a mechanical onset and implicates neurological involvement.
That he is unable to obtain full relief of pain when recumbent is of concern. It suggests a serious injury.
Are there any associated symptoms?
He says that a few hours after the injury he started experiencing difficulty to begin passing urine. He also notes that he has not been able to have a bowel motion for the past 2 days.
Analysis: Bladder and bowel dysfunction often are caused by nerve or muscle dysfunction. Other causes include medicinal side effects, stress, neurologic diseases, diabetes and pelvic floor disorders.
Is there a past history that is relevant to the current complaint?
He says that he has a long history of low back pain associated with his work as a carpenter. He has experienced some slight tingling in his lower extremities on some of those occasions but can’t remember whether it involved both legs. Each of the previous incidents has been relatively short-lived and he has found relief with manipulation and massage. The last bout was about 12 months ago and was the worst he had experienced. It took several weeks to settle and he had to see his medical practitioner who prescribed some anti-inflammatory medication. Radiographs were also taken at that time but he says they were described as “all clear”. He says that the severity of the symptoms on this occasion far exceed anything he has ever had in the past.
Analysis: The long history of back pain related to his carpentry work is not surprising. His past responses to conservative care would suggest a good prognosis. However, the severity of this recent episode, together with bilateral lower limb symptomatology, indicates that a different and more serious injury has occurred.
Are there any “red flags”?
The patient is asked the following questions in order to identify any “red flags” that could indicate serious pathology. Even if the patient has already provided information in the case history that relates to these questions, it is recommended that they be readdressed to ensure a thorough exploration.
Does your pain disappear even for a short time? “No. It’s always there.”
Does the pain wake you up at night? “I haven’t had a good night’s sleep for three nights. The pain just keeps going.”
Have you noticed any discoloration of your urine? “No.”
Have you had any bladder or bowel problems since the onset of your pain? “As I mentioned before, I have trouble beginning to pass urine and I haven’t been able to have a bowel movement since I hurt my back.”
Do you feel weak in your arms or legs? “I’m not sure. Maybe! I just can’t stand for too long. It hurts too much.”
Have you recently experienced any fever, chills, night sweats or vomiting? “No”.
Have you lost any weight recently? “No.”
Do you have a history of cancer or HIV? “No.”
Analysis: The patient’s responses raise “red flags”. One is the continuous nature of the pain, even when the patient is at rest, and the other is the urinary and bowel difficulties.
What is the list of possible causes for the patient’s complaint?
Based on the available history, the initial list of possible causes for the patient’s complaint includes:
• Posterocentral intervertebral disc herniation
• Cauda Equina Syndrome
• Neoplastic epidural spinal cord compression
• Vertebral metastases
• Pathological fracture
Reflection Points
Please stop and take a moment to consider whether the main requirements of an adequate and relevant patient history have been fulfilled. Are there any additional questions you would have asked and if so why?
Before the physical examination findings are presented below, please reflect on what physical examination procedures you would perform to adequately evaluate this patient.
Performing Physical Examination
In the sections below, you are provided with an example of physical examination findings for this patient. The material presents a systematic approach to performing a focused and relevant physical examination in order to narrow down the possible causes for the patient’s complaint. The material also provides ongoing clinical reasoning and analysis of the findings. As you read the following material you are encouraged to identify whether the essential elements of physical examination have been adequately covered.
Vital Signs
His vital signs are within normal limits.
Analysis: It is always important to examine the vital signs to screen the patient’s general health and help identify underlying conditions such as infection.
Inspection
The patient is in obvious distress and discomfort. His lumbar spine appears flattened and hypolordotic.
Analysis: The flattening of the lumbar spine in this patient is likely to be an antalgic response with or without muscle guarding.
Range of Motion
There is a global loss of active lumbar ranges of motion due to pain.
Analysis: The global loss of active lumbar ranges of motion due to pain is consistent with a significant injury to the lumbar spine.
Palpation
There is a diffuse tenderness on palpation throughout the lumbar spine, posterior pelvis and buttocks. Because of his pain and global loss of movement, it is not possible to perform a functional analysis of lumbar vertebral motion segments.
Analysis: The diffuse tenderness together with the significant loss of motion and severe pain indicate a serious underlying condition.
Neurological Examination
A neurological screening examination is performed and reveals the following:
• A significant loss of strength of ankle plantar-flexion bilaterally, but more pronounced on the right.
• A significant loss of sensation over the lateral side of the right heel and mild sensory loss on the same region on the left.
• Loss of sensation in the buttocks on both sides of the superior gluteal cleft, which is more pronounced on the right.
• Absent right Achilles reflex with a diminished reflex on the left.
Analysis: The findings on examination of muscle strength, sensation and reflexes are consistent with S1 nerve root involvement. The examination of the upper portion of the “saddle” area is consistent with saddle anesthesia involving S2 and S3 nerve roots.
Involvement of the S4 and S5 nerve roots is also possible but was not tested by this screening examination.
The results of the neurological examination are consistent with compression of the sacral nerve roots and with the development of Cauda Equina Syndrome.
Please watch the video below if you wish to view how a Neurological Screening Examination for Low Back Pain may be performed.
Reflection Point
Given the patient’s history and examination findings to this point please stop and take a moment to consider which special tests should be performed for this patient.
Special Tests
The Valsalva test is performed and is found to be positive, resulting in an increase in low back pain and pain and tingling in the lower extremities.
Analysis: A positive Valsalva test indicates the possibility of a space-occupying lesion. In this case, with bilateral lower limb symptomatology, a large central herniation of a disc or spinal hematoma should be considered. Please watch the video below if you wish to view how the Valsalva test is performed.
The Straight Leg Raise (SLR) test is performed bilaterally and reveals exacerbation of lower limb symptomatology at 40 degrees of elevation on each side.
Analysis: Bilateral lower limb radiculopathy is considered evidence of early-stage Cauda Equina Syndrome and indicates a high risk for the development of advanced Cauda Equina Syndrome. Please watch the video below if you wish to view how the SLR test is performed.
The Slump test is performed and reveals exacerbation of lower limb symptomatology bilaterally.
Analysis: The positive Slump test is further evidence for nerve root compression affecting both lower extremities. Please watch the video below if you wish to view how the Slump test is performed.
In light of the patient’s clinical findings to this point, you arrange for the patient to be taken to an emergency room for urgent MRI and specialist evaluation.
Reflection Point
Please stop and take a moment to consider whether all the elements of an adequate and relevant physical examination have been completed for this patient. Are there any additional procedures you would have performed and if so why?
Imaging
The patient’s MRI reveals a very large central disc extrusion at the L5-S1 level, compressing the cauda equina. The patient undergoes an urgent operation involving decompressive laminectomy and discectomy.

Diagnosis
Cauda Equina Syndrome
Discussion
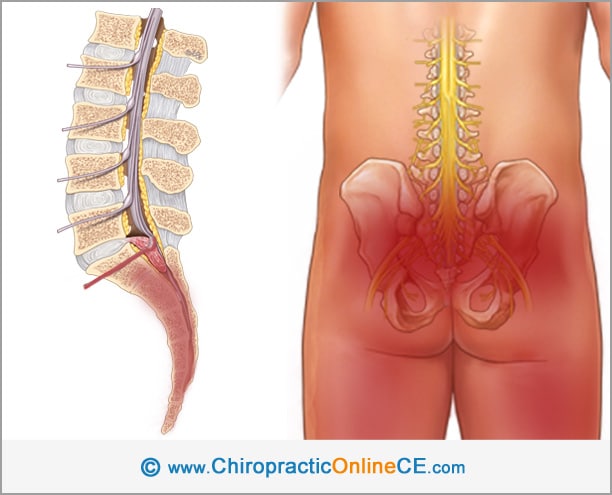
Cauda Equina Syndrome is a severe complication of lumbar spine disorders. The spinal cord ends at the level of the intervertebral disc between L1 and L2 as a tapered structure called the conus medullaris. Below the conus medullaris, the nerve roots extend downward in an array named the cauda equina. The cauda equina includes the nerve roots of L2 to L5 and all the sacral and coccygeal nerves.
Cauda Equina Syndrome results from compression of nerve roots of the cauda equina due to conditions such as:
• Centrally herniated discs
• Spinal tumors
• Spinal stenosis
• Infection or inflammation
• Fracture, dislocation or hematoma
Symptoms of Cauda Equina Syndrome include the following:
• Low back pain
• Unilateral or bilateral sciatica
• Saddle hypesthesia or anesthesia
• Bowel and bladder disturbances. Typically, urinary manifestations begin with urinary retention and are later followed by overflow urinary incontinence.
• Lower extremity motor weakness and sensory deficits
• Reduced or absent lower extremity reflexes
Cauda Equina Syndrome is rare but has serious consequences and can cause devastating long-lasting neurological deficits. Prompt evaluation and urgent Magnetic Resonance Imaging assessment should be performed in all patients who present with back pain in conjunction with sudden onset of urinary or bowel symptoms or abnormal neurological findings consistent with cauda equina involvement.
References and Suggested Further Readings:
McNamee J, Flynn P, O’Leary S, Love M, Kelly B. Imaging in Cauda Equina Syndrome – A Pictorial Review. Ulster Med J 2013;82(2):100-108
Raj D, Coleman N. Cauda equina syndrome secondary to lumbar disc herniation. Acta Orthop Belg. 2008 Aug. 74(4):522-7.
Olivero W, Wang H, Hanigan W, Henderson J; Tracy P, Elwood P, Lister R, Lyleet L. Cauda Equina Syndrome (CES) From Lumbar Disc Herniations. Journal of Spinal Disorders & Techniques. 22(3):202-206, MAY 2009
Majlesi J, Togay H, Ünalan H, Toprak S. The sensitivity and specificity of the Slump and the Straight Leg Raising tests in patients with lumbar disc herniation. J Clin Rheumatol. 2008 Apr;14(2):87-91.
Mauffrey C, Randhawa K, Lewis C, Brewster M, Dabke H. Cauda equina syndrome: an anatomically driven review. Br J Hosp Med (Lond). 2008 Jun. 69(6):344-7.
Schiff D. Clinical features and diagnosis of neoplastic epidural spinal cord compression, including cauda equina syndrome. www.uptodate.com
Dawodu S. Cauda Equina and Conus Medullaris Syndromes. www.emedicine.medscape.com
Mauffrey C, Randhawa K, Lewis C, Brewster M, Dabke H. Cauda equina syndrome: an anatomically driven review. Br J Hosp Med (Lond). 2008 Jun. 69(6):344-7.
Panos et al. Differential diagnosis and treatment of acute cauda equina syndrome in the human immunodeficiency virus positive patient: a case report and review of the literature. Journal of Medical Case Reports (2016) 10:165
This concludes the learning material for unit 1.
Thank you for Reviewing this Free Sample.
This unit also has a 5 question multiple-choice quiz. The quiz is not included in this free sample. Please note that the quiz questions are directly from the content of this unit. You can attempt the quiz as many times as you need to achieve a pass mark of at least 60%.